Ebola Virus Disease From Wikipedia, the free encyclopedia
SSTattler: This is For Your Information For Stroke Survivors - an epidemic of Ebola virus disease (EVD) is ongoing in West Africa events in 2014 West Africa Ebola virus outbreak; but two case in the US; and one (maybe more) in Spain. Read at least this blog below or on TV or on Radio. |
| Ebola Virus Disease A 1976 photograph of two nurses standing in front of Mayinga N., a person with Ebola virus disease; she died only a few days later due to severe internal hemorrhaging. |
The virus may be acquired upon contact with blood or bodily fluids of an infected human or other animal. Spreading through the air has not been documented in the natural environment. Fruit bats are believed to be a carrier and may spread the virus without being affected. Once human infection occurs, the disease may spread between people, as well. Male survivors may be able to transmit the disease via semen for nearly two months. To make the diagnosis, typically other diseases with similar symptoms such as malaria, cholera and other viral hemorrhagic fevers are first excluded. To confirm the diagnosis, blood samples are tested for viral antibodies, viral RNA, or the virus itself.
Outbreak control require community engagement, case management, surveillance and contact tracing, a good laboratory service, and safe burials. Prevention includes decreasing the spread of disease from infected animals to humans. This may be done by checking such animals for infection and killing and properly disposing of the bodies if the disease is discovered. Properly cooking meat and wearing protective clothing when handling meat may also be helpful, as are wearing protective clothing and washing hands when around a person with the disease. Samples of bodily fluids and tissues from people with the disease should be handled with special caution.
No specific treatment for the disease is yet available. Efforts to help those who are infected are supportive and include giving either oral rehydration therapy (slightly sweet and salty water to drink) or intravenous fluids. This supportive care improves outcomes. The disease has a high risk of death, killing between 50% and 90% of those infected with the virus. EVD was first identified in an area of Sudan that is now part of South Sudan, as well as in Zaire (now the Democratic Republic of the Congo). The disease typically occurs in outbreaks in tropical regions of sub-Saharan Africa. From 1976 (when it was first identified) through 2013, the World Health Organization reported a total of 1,716 cases. The largest outbreak to date is the ongoing 2014 West African Ebola outbreak, which is affecting Guinea, Sierra Leone, Liberia, and Nigeria. As of 28 September 2014, 7,157 suspected cases resulting in the deaths of 3,330 have been reported. Efforts are under way to develop a vaccine; however, none yet exists.
Signs and Symptoms
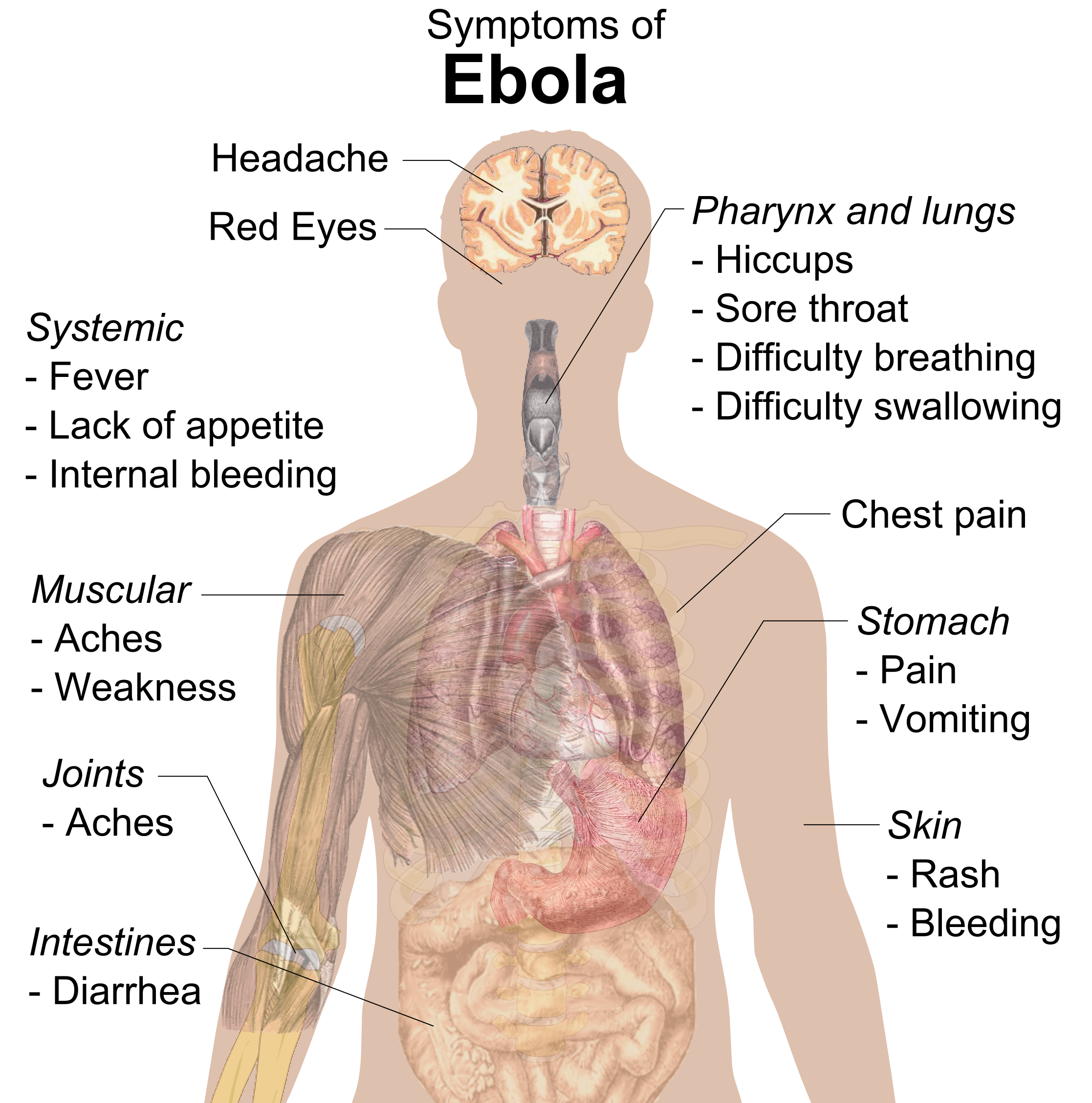 |
| Signs and symptoms of Ebola. |
In 40–50% of cases, bleeding from puncture sites and mucous membranes (e.g., gastrointestinal tract, nose, vagina, and gums) has been reported. In the bleeding phase, which typically begins five to seven days after first symptoms, internal and subcutaneous bleeding may present itself in the form of reddened eyes and bloody vomit. Bleeding into the skin may create petechiae, purpura, ecchymoses, and hematomas (especially around needle injection sites). Sufferers may cough up blood, vomit it, or excrete it in their stool.
Heavy bleeding is rare and is usually confined to the gastrointestinal tract. In general, the development of bleeding symptoms often indicates a worse prognosis and this blood loss can result in death. All people infected show some signs of circulatory system involvement, including impaired blood clotting. If the infected person does not recover, death due to multiple organ dysfunction syndrome occurs within 7 to 16 days (usually between days 8 and 9) after first symptoms.
Causes
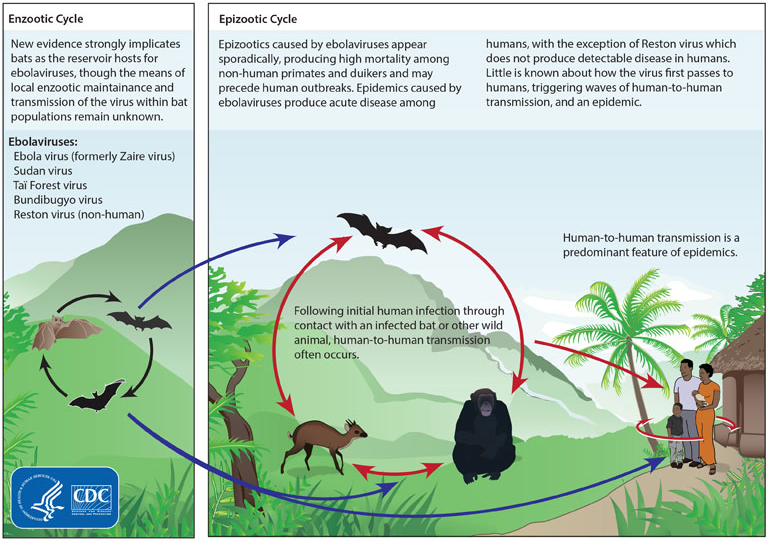 |
| Life cycles of the Ebolavirus |
Transmission
Human-to-human transmission can occur via direct contact with blood or bodily fluids from an infected person (including embalming of an infected dead person) or by contact with objects contaminated by the virus, particularly needles and syringes. Other body fluids with ebola virus include saliva, mucus, vomit, feces, sweat, tears, breast milk, urine, and semen. Entry points include the nose, mouth, eyes, or open wounds, cuts and abrasions. The potential for widespread EVD infections is considered low as the disease is only spread by direct contact with the secretions from someone who is showing signs of infection. The symptoms limit a person's ability to spread the disease as they are often too sick to travel. Because dead bodies are still infectious, traditional burial rituals may spread the disease. Nearly two thirds of the cases of Ebola in Guinea during the 2014 outbreak are believed to be due to burial practices. Semen may be infectious in survivors for up to 3 months. It is not entirely clear how an outbreak is initially started. The initial infection is believed to occur after ebola virus is transmitted to a human by contact with an infected animal's body fluids.
One of the primary reasons for spread is that the health systems in the part of Africa where the disease occurs function poorly. Medical workers who do not wear appropriate protective clothing may contract the disease. Hospital-acquired transmission has occurred in African countries due to the reuse of needles and lack of universal precautions. Some healthcare centers caring for people with the disease do not have running water.
Airborne transmission has not been documented during EVD outbreaks. They are, however, infectious as breathable 0.8– to 1.2-μm laboratory-generated droplets. The virus has been shown to travel, without contact, from pigs to primates, although the same study failed to demonstrate similar transmission between non-human primates.
Bats drop partially eaten fruits and pulp, then land mammals such as gorillas and duikers feed on these fallen fruits. This chain of events forms a possible indirect means of transmission from the natural host to animal populations, which has led to research towards viral shedding in the saliva of bats. Fruit production, animal behavior, and other factors vary at different times and places that may trigger outbreaks among animal populations.
Reservoir
| Bushmeat being prepared for cooking in Ghana, 2013. Human consumption of equatorial animals in Africa in the form of bushmeat has been linked to the transmission of diseases to people, including Ebola. |
Between 1976 and 1998, in 30,000 mammals, birds, reptiles, amphibians and arthropods sampled from outbreak regions, no ebolavirus was detected apart from some genetic traces found in six rodents (Mus setulosus and Praomys) and one shrew (Sylvisorex ollula) collected from the Central African Republic. Traces of EBOV were detected in the carcasses of gorillas and chimpanzees during outbreaks in 2001 and 2003, which later became the source of human infections. However, the high lethality from infection in these species makes them unlikely as a natural reservoir.
Transmission between natural reservoir and humans is rare, and outbreaks are usually traceable to a single case where an individual has handled the carcass of gorilla, chimpanzee or duiker. Fruit bats are also eaten by people in parts of West Africa where they are smoked, grilled or made into a spicy soup.
Virology
Genome
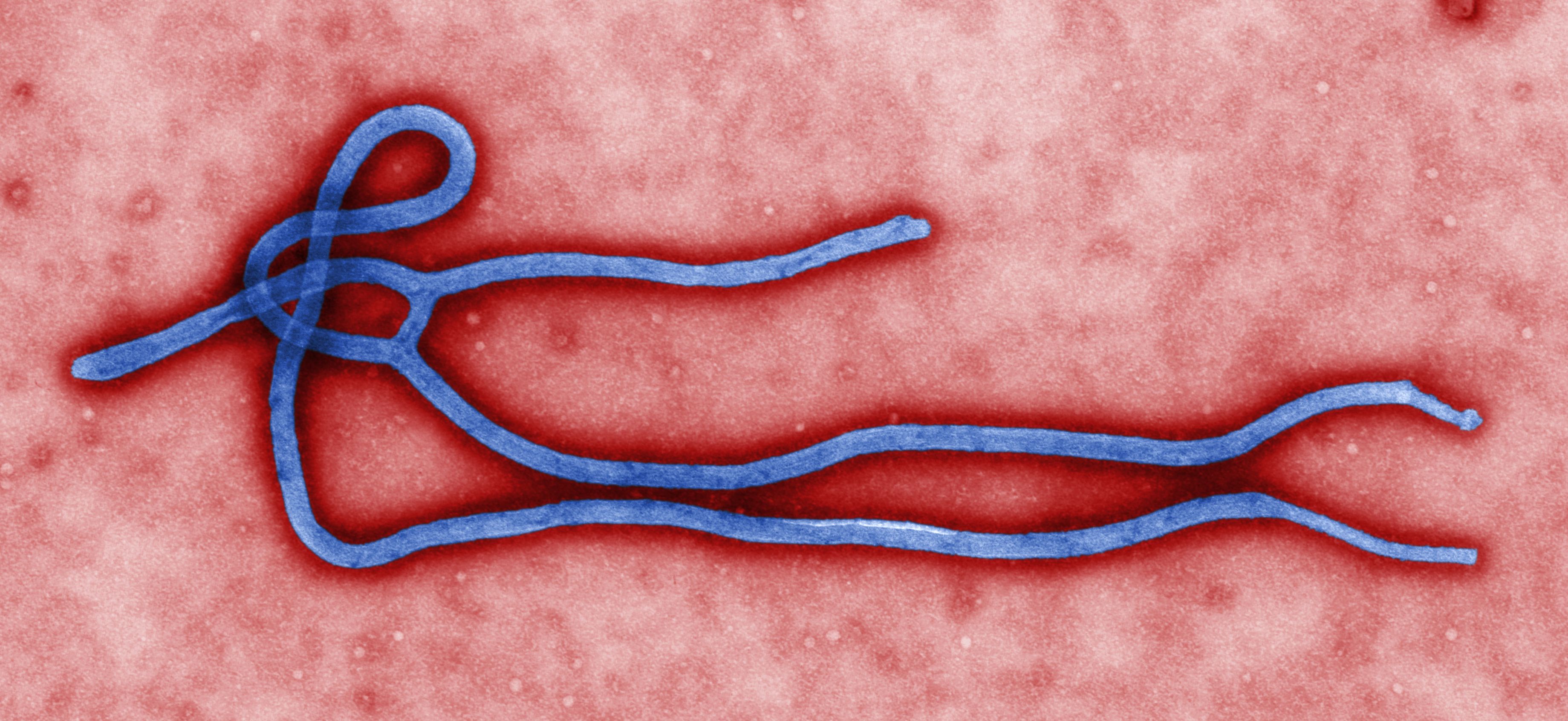 |
| Electron micrograph of an Ebola virus virion |
Structure
Like all filoviruses, ebolavirions are filamentous particles that may appear in the shape of a shepherd's crook or in the shape of a "U" or a "6", and they may be coiled, toroid, or branched. In general, ebolavirions are 80 nm in width, but vary somewhat in length. In general, the median particle length of ebolaviruses ranges from 974 to 1,086 nm (in contrast to marburgvirions, whose median particle length was measured at 795–828 nm), but particles as long as 14,000 nm have been detected in tissue culture.
Replication
The ebolavirus life cycle begins with virion attachment to specific cell-surface receptors, followed by fusion of the virion envelope with cellular membranes and the concomitant release of the virus nucleocapsid into the cytosol. The viral RNA polymerase, encoded by the L gene, partially uncoats the nucleocapsid and transcribes the genes into positive-strand mRNAs, which are then translated into structural and nonstructural proteins. Ebolavirus RNA polymerase (L) binds to a single promoter located at the 3' end of the genome. Transcription either terminates after a gene or continues to the next gene downstream. This means that genes close to the 3' end of the genome are transcribed in the greatest abundance, whereas those toward the 5' end are least likely to be transcribed. The gene order is, therefore, a simple but effective form of transcriptional regulation. The most abundant protein produced is the nucleoprotein, whose concentration in the cell determines when L switches from gene transcription to genome replication. Replication results in full-length, positive-strand antigenomes that are, in turn, transcribed into negative-strand virus progeny genome copy. Newly synthesized structural proteins and genomes self-assemble and accumulate near the inside of the cell membrane. Virions bud off from the cell, gaining their envelopes from the cellular membrane they bud from. The mature progeny particles then infect other cells to repeat the cycle. The Ebola virus genetics are difficult to study due to its virulent nature.
Pathophysiology
| Pathogenesis schematic |
The presence of viral particles and cell damage resulting from budding causes the release of chemical signals (to be specific, TNF-α, IL-6, IL-8, etc.), which are the signaling molecules for fever and inflammation. The cytopathic effect, from infection in the endothelial cells, results in a loss of vascular integrity. This loss in vascular integrity is furthered with synthesis of GP, which reduces specific integrins responsible for cell adhesion to the inter-cellular structure, and damage to the liver, which leads to improper clotting.
Diagnosis
The travel and work history along with exposure to wildlife are important to consider when the diagnosis of EVD is suspected. The diagnosis is confirmed by isolating the virus, detecting its RNA or proteins, or detecting antibodies against the virus in a person's blood. Isolating the virus by cell culture, detecting the viral RNA by polymerase chain reaction (PCR) and detecting proteins by enzyme-linked immunosorbent assay (ELISA) works best early and in those who have died from the disease. Detecting antibodies against the virus works best late in the disease and in those who recover.
During an outbreak, virus isolation is often not feasible. The most common diagnostic methods are therefore real-time PCR and ELISA detection of proteins, which can be performed in field or mobile hospitals. Filovirions can be seen and identified in cell culture by electron microscopy due to their unique filamentous shapes, but electron microscopy cannot tell the difference between the various filoviruses despite there being some length differences.
Classification
| Phylogenetic tree comparing the Ebolavirus and Marburgvirus. Numbers indicate percent confidence of branches. |
Rates of genetic change are 100 times slower than influenza A in humans, but on the same magnitude as those of hepatitis B. Extrapolating backwards using these rates indicates that Ebolavirus and Marburgvirus diverged several thousand years ago. However, paleoviruses (genomic fossils) of filoviruses (Filoviridae) found in mammals indicate that the family itself is at least tens of millions of years old. Fossilized viruses that are closely related to ebolaviruses have been found in the genome of the Chinese hamster.
Differential Diagnosis
The symptoms of EVD are similar to those of Marburg virus disease. It can also easily be confused with many other diseases common in Equatorial Africa such as other viral hemorrhagic fevers, falciparum malaria, typhoid fever, shigellosis, rickettsial diseases such as typhus, cholera, gram-negative septicemia, borreliosis such as relapsing fever or EHEC enteritis. Other infectious diseases that should be included in the differential diagnosis include the following: leptospirosis, scrub typhus, plague, Q fever, candidiasis, histoplasmosis, trypanosomiasis, visceral leishmaniasis, hemorrhagic smallpox, measles, and fulminant viral hepatitis. Non-infectious diseases that can be confused with EVD are acute promyelocytic leukemia, hemolytic uremic syndrome, snake envenomation, clotting factor deficiencies/platelet disorders, thrombotic thrombocytopenic purpura, hereditary hemorrhagic telangiectasia, Kawasaki disease, and even warfarin poisoning.
Prevention
Infection Control and Containment
 |
| A researcher working with the Ebola virus while wearing a BSL-4 positive pressure suit to avoid infection |
In order to reduce the spread, the World Health Organization recommends raising community awareness of the risk factors for Ebola infection and the protective measures individuals can take. These include avoiding contact with infected people and regular hand washing using soap and water. Traditional burial rituals, especially those requiring washing or embalming of bodies, should be discouraged or modified. Social anthropologists may help find alternatives to traditional rules for burials. Airline crews are instructed to isolate anyone who has symptoms resembling Ebola virus.
The Ebola virus can be eliminated with heat (heating for 30 to 60 minutes at 60 °C or boiling for 5 minutes). On surfaces, some lipid solvents such as some alcohol-based products, detergents, sodium hypochlorite (bleach) or calcium hypochlorite (bleaching powder), and other suitable disinfectants at appropriate concentrations can be used as disinfectants.
In laboratories where diagnostic testing is carried out, biosafety level 4-equivalent containment is required, since Ebola viruses are World Health Organization Risk Group 4 pathogens. Laboratory researchers must be properly trained in BSL-4 practices and wear proper personal protective equipment.
Quarantine
Quarantine, also known as enforced isolation, is usually effective in decreasing spread. Governments often quarantine areas where the disease is occurring or individuals who may be infected. In the United States, the law allows quarantine of those infected with Ebola. During the 2014 outbreak, Liberia closed schools.
Contact Tracing
Contact tracing is regarded as important to contain an outbreak. It involves finding everyone who had close contact with infected individuals and watching for signs of illness for 21 days. If any of these contacts comes down with the disease, they should be isolated, tested, and treated. Then repeat the process by tracing the contacts' contacts.
Treatment
Standard Support
 |
| A hospital isolation ward in Gulu, Uganda, during the October 2000 outbreak |
Intensive Care
Intensive care is often used in the developed world. This may include maintaining blood volume and electrolytes (salts) balance as well as treating any bacterial infections that may develop. Dialysis may be needed for kidney failure while extracorporeal membrane oxygenation may be used for lung dysfunction.
Prognosis
The disease has a high mortality rate: often between 25 percent and 90 percent. As of September 2014, information from WHO across all occurrences to date puts the overall fatality rate at 50%. There are indications based on variations in death rate between countries that early and effective treatment of symptoms (e.g., supportive care to prevent dehydration) may reduce the fatality rate significantly. If an infected person survives, recovery may be quick and complete. Prolonged cases are often complicated by the occurrence of long-term problems, such as inflammation of the testicles, joint pains, muscle pains, skin peeling, or hair loss. Eye symptoms, such as light sensitivity, excess tearing, iritis, iridocyclitis, choroiditis, and blindness have also been described. EBOV and SUDV may be able to persist in the semen of some survivors for up to seven weeks, which could give rise to infections and disease via sexual intercourse.
Epidemiology
 |
| CDC worker incinerates medical waste from Ebola patients in Zaire in 1976 |
1976
The first identified case of Ebola was on 26 August 1976, in Yambuku, a small rural village in Mongala District in northern Democratic Republic of the Congo (then known as Zaire). The first victim, and the index case for the disease, was village school headmaster Mabalo Lokela, who had toured an area near the Central African Republic border along the Ebola river between 12–22 August. On 8 September he died of what would become known as the Ebola virus species of the ebolavirus. Subsequently a number of other cases were reported, almost all centered on the Yambuku mission hospital or having close contact with another case. 318 cases and 280 deaths (a 88% fatality rate) occurred in the DRC. The Ebola outbreak was contained with the help of the World Health Organization and transport from the Congolese air force, by quarantining villagers, sterilizing medical equipment, and providing protective clothing. The virus responsible for the initial outbreak, first thought to be Marburg virus, was later identified as a new type of virus related to Marburg, and named after the nearby Ebola river. Another ebolavirus, the Sudan virus species, was also identified that same year when an outbreak occurred in Sudan, affecting 284 people and killing 151.
1995 to 2013
The second major outbreak occurred in 1995 in the Democratic Republic of Congo, affecting 315 and killing 254. The next major outbreak occurred in Uganda in 2000, affecting 425 and killing 224; in this case the Sudan virus was found to be the ebolavirus species responsible for the outbreak. In 2003 there was an outbreak in the Republic of Congo that affected 143 and killed 128, a death rate of 90%, the highest to date.
In August 2007, 103 people were infected by a suspected hemorrhagic fever outbreak in the village of Kampungu, Democratic Republic of the Congo. The outbreak started after the funerals of two village chiefs, and 217 people in four villages fell ill. The 2007 outbreak eventually affected 264 individuals and resulted in the deaths of 187.
On 30 November 2007, the Uganda Ministry of Health confirmed an outbreak of Ebola in the Bundibugyo District in Western Uganda. After confirmation of samples tested by the United States National Reference Laboratories and the Centers for Disease Control, the World Health Organization confirmed the presence of a new species of Ebolavirus, which was tentatively named Bundibugyo. The WHO reported 149 cases of this new strain and 37 of those led to deaths.
The WHO confirmed two small outbreaks in Uganda in 2012. The first outbreak affected 7 people and resulted in the death of 4 and the second affected 24, resulting in the death of 17. The Sudan variant was responsible for both outbreaks.
On 17 August 2012, the Ministry of Health of the Democratic Republic of the Congo reported an outbreak of the Ebola-Bundibugyo variant in the eastern region. Other than its discovery in 2007, this was the only time that this variant has been identified as the ebolavirus responsible for an outbreak. The WHO revealed that the virus had sickened 57 people and claimed 29 lives. The probable cause of the outbreak was tainted bush meat hunted by local villagers around the towns of Isiro and Viadana.
2014 Outbreak
Main article: 2014 West Africa Ebola virus outbreak.
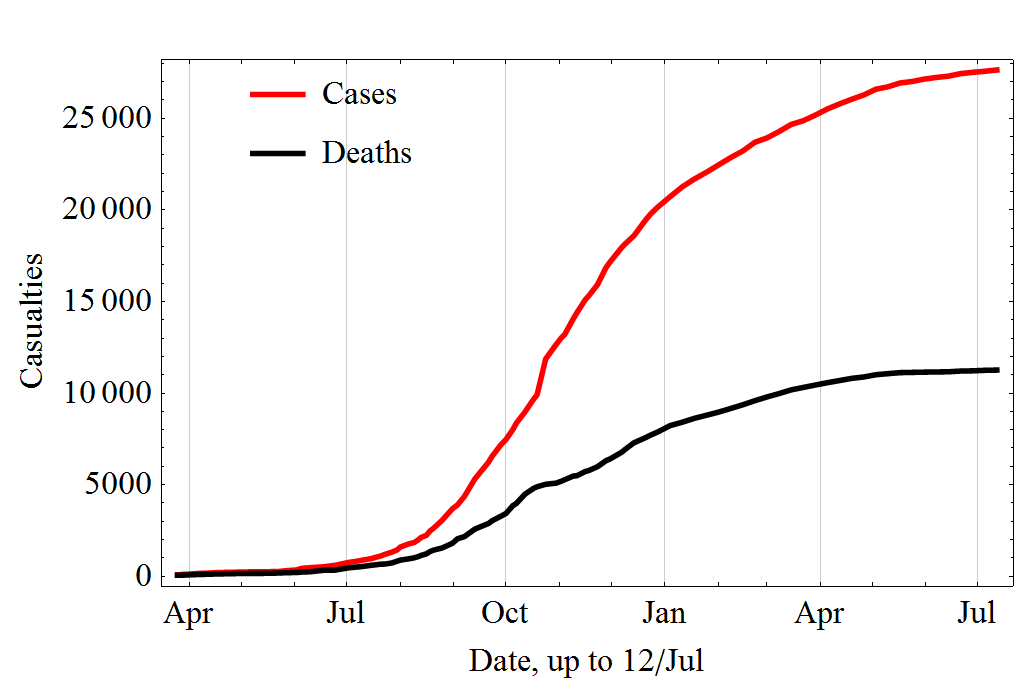 |
| Increase over time in the cases and deaths during the 2014 outbreak |
On 8 August 2014, the WHO declared the epidemic to be an international public health emergency. Urging the world to offer aid to the affected regions, the Director-General said, "Countries affected to date simply do not have the capacity to manage an outbreak of this size and complexity on their own. I urge the international community to provide this support on the most urgent basis possible." By mid-August 2014, Doctors Without Borders reported the situation in Liberia's capital Monrovia as "catastrophic" and "deteriorating daily". They reported that fears of Ebola among staff members and patients had shut down much of the city’s health system, leaving many people without treatment for other conditions. By late August 2014, the disease had spread to Nigeria, and one case was reported in Senegal. On 30 September 2014, the first confirmed case of Ebola was diagnosed in the United States at Texas Health Presbyterian Hospital in Dallas, Texas.
Aside from the human cost, the outbreak has severely eroded the economies of the affected countries. A Financial Times report suggested the economic impact of the outbreak could kill more people than the virus itself. As of 23 September, in the three hardest hit countries, Liberia, Sierra Leone, and Guinea, there were only 893 treatment beds available while the current need was 2122. In a 26 September statement, the WHO said, "The Ebola epidemic ravaging parts of West Africa is the most severe acute public health emergency seen in modern times. Never before in recorded history has a biosafety level four pathogen infected so many people so quickly, over such a broad geographical area, for so long."
By 29 September 2014, 7,192 suspected cases and 3,286 deaths had been reported, however the World Health Organization has said that these numbers may be vastly underestimated. The WHO reports that more than 216 healthcare workers are among the dead, partly due to the lack of equipment and long hours.
History
 |
| Cases of ebola fever in Africa from 1979 to 2008. |
In late 1989, Hazelton Research Products' Reston Quarantine Unit in Reston, Virginia suffered a mysterious outbreak of fatal illness (initially diagnosed as Simian hemorrhagic fever virus (SHFV)) among a shipment of crab-eating macaque monkeys imported from the Philippines. Hazelton's veterinary pathologist sent tissue samples from dead animals to the United States Army Medical Research Institute of Infectious Diseases (USAMRIID) at Fort Detrick, Maryland, where a laboratory test known as an ELISA assay showed antibodies to Ebola virus. An electron microscopist from USAMRIID discovered filoviruses similar in appearance to Ebola in the tissue samples sent from Hazelton Research Products' Reston Quarantine Unit.
Shortly afterward, a US Army team headquartered at USAMRIID went into action to euthanize the monkeys which had not yet died, bringing those monkeys and those which had already died of the disease to Ft. Detrick for study by the Army's veterinary pathologists and virologists, and eventual disposal under safe conditions.
Blood samples were taken from 178 animal handlers during the incident. Of those, six animal handlers eventually seroconverted, including one who had cut himself with a bloody scalpel. When the handlers did not become ill, the CDC concluded that the virus had a very low pathogenicity to humans.
The Philippines and the United States had no previous cases of Ebola infection, and upon further isolation, researchers concluded it was another strain of Ebola, or a new filovirus of Asian origin, which they named Reston ebolavirus (REBOV) after the location of the incident.
Society and Culture
Ebolavirus is classified as a biosafety level 4 agent, as well as a Category A bioterrorism agent by the Centers for Disease Control and Prevention. It has the potential to be weaponized for use in biological warfare, and was investigated by the Biopreparat for such use, but might be difficult to prepare as a weapon of mass destruction because the virus becomes ineffective quickly in open air.
Literature
Richard Preston's 1995 best-selling book, The Hot Zone, dramatized the Ebola outbreak in Reston, Virginia.
William Close's 1995 Ebola: A Documentary Novel of Its First Explosion and 2002 Ebola: Through the Eyes of the People focused on individuals' reactions to the 1976 Ebola outbreak in Zaire.
Tom Clancy's 1996 novel, Executive Orders, involves a Middle Eastern terrorist attack on the United States using an airborne form of a deadly Ebola virus strain named "Ebola Mayinga" (see Mayinga N'Seka).
Other Animals
Wild Animals
It is widely believed that outbreaks of EVD among human populations result from handling infected wild animal carcasses. Some research suggests that an outbreak in the wild animals used for consumption, bushmeat, may result in a corresponding human outbreak. Since 2003, such outbreaks have been monitored through surveillance of animal populations with the aim of predicting and preventing Ebola outbreaks in humans.
Recovered carcasses from gorillas contain multiple Ebola virus strains, which suggest multiple introductions of the virus. Bodies decompose quickly and carcasses are not infectious after three to four days. Contact between gorilla groups is rare, suggesting transmission among gorilla groups is unlikely, and that outbreaks result from transmission between viral reservoir and animal populations.
Ebola has a high mortality among primates. Frequent outbreaks of Ebola may have resulted in the deaths of 5,000 gorillas. Outbreaks of Ebola may have been responsible for an 88% decline in tracking indices of observed chimpanzee populations in 420 square kilometer Lossi Sanctuary between 2002 and 2003. Transmission among chimpanzees through meat consumption constitutes a significant risk factor, while contact between individuals, such as touching dead bodies and grooming, is not.
Domesticated Animals
Reston ebolavirus (REBOV) can be transmitted to pigs. This virus was discovered during an outbreak of what at the time was thought to be simian hemorrhagic fever virus (SHFV) in crab-eating macaques in Reston, Virginia (hence the name Reston elabavirus) in 1989. Since the initial outbreak it has since been found in nonhuman primates in Pennsylvania, Texas, and Italy. In each case, the affected animals had been imported from a facility in the Philippines, where the virus had infected pigs. Despite its status as a Level‑4 organism and its apparent pathogenicity in monkeys, REBOV has not caused disease in exposed human laboratory workers. In 2012 it was demonstrated that the virus can travel without contact from pigs to nonhuman primates, although the same study failed to achieve transmission in that manner between primates. According to the WHO, routine cleaning and disinfection of pig (or monkey) farms with sodium hypochlorite or other detergents should be effective in inactivating the Reston ebolavirus. If an outbreak is suspected, the area must be immediately quarantined.
While pigs that have been infected with REBOV tend to show symptoms of the disease, it has been shown that dogs may become infected with EBOV and remain asymptomatic. Dogs in some parts of Africa scavenge for their food and it is known that they sometimes eat infected animals and the corpses of humans. Although they remain asymptomatic, a 2005 survey of dogs during an EBOV outbreak found that over 31.8% showed a seroprevalence for EBOV closest to an outbreak versus 9% a farther distance away.
Research
A number of experimental treatments are being studied. In the United States, the Food and Drug Administration (FDA)'s animal efficacy rule is being used to demonstrate reasonable safety to obtain permission to treat people who are infected with Ebola. It is being used as the normal path for testing drugs is not possible for diseases caused by dangerous pathogens or toxins. Experimental drugs are made available for use with the approval of regulatory agencies under named patient programs, known in the US as "expanded access". On 12 August the WHO released a statement that the use of not yet proven treatments is ethical in certain situations in an effort to treat or prevent the disease.
Medications
 |
| Researchers looking at slides of cultures of cells that make monoclonal antibodies. These are grown in a lab and the researchers are analyzing the products to select the most promising of them. |
The FDA has allowed three drugs: ZMapp, an RNA interference drug called TKM-Ebola, and brincidofovir to be used in people infected with Ebola under these programs during the 2014 outbreak. BioCryst's BCX4430 small molecule is undergoing further animal testing as a possible therapy in humans. Another drug favipiravir has been used with apparent success in a patient medically evacuated to France.
ZMapp is a monoclonal antibody vaccine. The limited supply of the drug has been used to treat a small number of individuals infected with the Ebola virus. Although some of these have recovered the outcome is not considered statistically significant. ZMapp has proved effective in a trial involving Rhesus macaque monkeys.
Antivirals
A number of antiviral medications are being studied. Favipiravir, an anti-viral drug approved in Japan for stockpiling against influenza pandemics, appears to be useful in a mouse model of Ebola. On 4 October 2014, it was reported that a French nun who contracted Ebola while volunteering in Liberia was cured with Favipiravir treatment. BCX4430 is a broad-spectrum antiviral drug developed by BioCryst Pharmaceuticals and currently being researched as a potential treatment for Ebola by USAMRIID. The drug has been approved to progress to Phase 1 trials, expected late in 2014. Brincidofovir, another broad-spectrum antiviral drug, has been granted an emergency FDA approval as an investigational new drug for the treatment of Ebola, after it was found to be effective against Ebolavirus in in vitro tests. It has subsequently been used to treat the first patient diagnosed with Ebola in the USA, after he had recently returned from Liberia. The antiviral drug lamivudine, which is usually used to treat HIV / AIDS, was reported in September 2014 to have been used successfully to treat 13 out of 15 Ebola-infected patients by a doctor in Liberia, as part of a combination therapy also involving intravenous fluids and antibiotics to combat opportunistic bacterial infection of Ebola-compromised internal organs. Western virologists have however expressed caution about the results, due to the small number of patients treated and confounding factors present. Researchers at the NIH stated that lamivudine had so far failed to demonstrate anti-Ebola activity in preliminary in vitro tests, but that they would continue to test it under different conditions and would progress it to trials if even slight evidence for efficacy is found.
Antisense Technology
Other promising treatments rely on antisense technology. Both small interfering RNAs (siRNAs) and phosphorodiamidate morpholino oligomers (PMOs) targeting the Zaire Ebola virus (ZEBOV) RNA polymerase L protein could prevent disease in nonhuman primates. TKM-Ebola is a small-interfering RNA compound, currently being tested in a Phase I clinical trial in humans. Sarepta Therapeutics has completed a Phase I clinical trial with its Morpholino oligo targeting Ebola.
Other
Two selective estrogen receptor modulators used to treat infertility and breast cancer (clomiphene and toremifene) have been found to inhibit the progress of Ebola virus in infected mice. Ninety percent of the mice treated with clomiphene and fifty percent of those treated with toremifene survived the tests.
A 2014 study found that three ion channel blockers used in the treatment of heart arrhythmias, amiodarone, dronedarone and verapamil, block the entry of Ebolavirus into cells in vitro. Given their oral availability and history of human use, these drugs would be candidates for treating Ebola virus infection in remote geographical locations, either on their own or together with other antiviral drugs.
Melatonin has also been suggested as a potential treatment for Ebola based on promising in vitro results.
Blood Products
The WHO has stated that transfusion of whole blood or purified serum from Ebola survivors is the therapy with the greatest potential to be implemented immediately, although there is little information as to its efficacy. At the end of September, WHO issued an interim guideline for this therapy. The blood serum from those who have survived an infection is currently being studied to see if it is an effective treatment. During a meeting arranged by WHO this research was deemed to be a top priority. Seven of eight people with Ebola survived after receiving a transfusion of blood donated by individuals who had previously survived the infection in an 1999 outbreak in the Democratic Republic of the Congo. This treatment, however, was started late in the disease meaning they may have already been recovering on their own and the rest of their care was better than usual. Thus this potential treatment remains controversial. Intravenous antibodies appear to be protective in non-human primates who have been exposed to large doses of Ebola. The World Health Organisation has approved the use of convalescent serum and whole blood products to treat people with Ebola.
Vaccine
As of September 2014, no vaccine was approved for clinical use in humans. It was hoped that one would be initially available by November 2014. The most promising candidates are DNA vaccines or vaccines derived from adenoviruses, vesicular stomatitis Indiana virus (VSIV) or filovirus-like particles (VLPs) because these candidates could protect nonhuman primates from ebolavirus-induced disease. DNA vaccines, adenovirus-based vaccines, and VSIV-based vaccines have entered clinical trials.
Vaccines have protected nonhuman primates. Immunization takes six months, which impedes the counter-epidemic use of the vaccines. Searching for a quicker onset of effectiveness, in 2003, a vaccine using an adenoviral (ADV) vector carrying the Ebola spike protein was tested on crab-eating macaques. Twenty-eight days later, they were challenged with the virus and remained resistant. A vaccine based on attenuated recombinant vesicular stomatitis virus (VSV) vector carrying either the Ebola glycoprotein or the Marburg glycoprotein in 2005 protected nonhuman primates, opening clinical trials in humans. The study by October completed the first human trial, over three months giving three vaccinations safely inducing an immune response. Individuals for a year were followed, and, in 2006, a study testing a faster-acting, single-shot vaccine began; this new study was completed in 2008. Trying the vaccine on a strain of Ebola that more resembles one that infects humans is the next step. On 6 December 2011, the development of a successful vaccine against Ebola for mice was reported. Unlike the predecessors, it can be freeze-dried and thus stored for long periods in wait for an outbreak. An experimental vaccine made by researchers at Canada's national laboratory in Winnipeg was used, in 2009, to pre-emptively treat a German scientist who might have been infected during a lab accident. However, actual EBOV infection was never demonstrated beyond doubt. Experimentally, recombinant vesicular stomatitis Indiana virus (VSIV) expressing the glycoprotein of EBOV or SUDV has been used successfully in nonhuman primate models as post-exposure prophylaxis. The CDC's recommendations are currently under review.[citation needed]
Simultaneous phase 1 trials of an experimental vaccine known as the NIAID/GSK vaccine commenced in September 2014. GlaxoSmithKline and the NIH jointly developed the vaccine, based on a modified chimpanzee adenovirus, and contains parts of the Zaire and Sudan ebola strains. If this phase is completed successfully, the vaccine will be fast tracked for use in West Africa. In preparation for this, GSK is preparing a stockpile of 10,000 doses.
See the full article:
Ebola Virus Disease From Wikipedia, the free encyclopedia

No comments:
Post a Comment