Hocoma From Wikipedia, the free encyclopedia.
Robotic Rehabilitation, Medical technology Volketswil, Switzerland
Hocoma is a privately hold globally active medical technology company based near Zurich, Switzerland. Hocoma was founded in 2000 as spin-off of the Spinal Cord Injury Center of the Balgrist University Hospital in Zurich, by the electrical and biomedical engineers Gery Colombo and Matthias Jörg and the economist Peter Hostettler. Today, Hocoma employs more than 110 people at its headquarter near Zurich and in its subsidiaries in Norwell, Massachusetts and Singapore. It develops therapy solutions for neurorehabilitation and low back pain therapy working closely with clinics and research centers. The Hocoma therapy solutions support the treatment of neurological patients with movement disorders caused by stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, cerebral palsy or other neurological diseases and injuries as well as low back pain patients.
Lokomat
The Lokomat is a gait therapy device on a treadmill with a robotic gait orthosis, and exercises in a virtual reality environment with a constant audio and visual feedback. The Lokomat also provides a pediatric orthosis for driven locomotion therapy for small children. The enhanced efficiency and efficacy of locomotion training with the Lokomat has been scientifically proven in over 100 publications in peer reviewed journals. That is more than any other robotic therapy device for lower extremity rehabilitation.In 2011, U.S. News & World Report surveyed almost 5000 hospitals in the US and ranked them in 16 specialties. Nine out of ten hospitals ranked as the top ten in “Rehabilitation” offer gait therapy with Hocoma’s Lokomat. By the end of 2011, over 390 Lokomat devices were in clinical usages in hospitals and clinics worldwide.
Other products: Armeo Therapy Concept, Erigo, and Valedo.
See the full article Hocoma From Wikipedia, the free encyclopedia.
Lokomat Product Demonstration
Uploaded on Oct 3, 2010Find out more at http://www.evolutionofjeff.com.
The Lokomat is the device that started Jeff's new journey. At the Rehabilitation Institute of Chicago, he was harnessed to the ceiling and lowered into the device with his son, Zack, looking on. Produced by Swiss robotic rehabilitation firm Hocoma, the machine is meant for "neurological patients with movement disorders caused by stroke, spinal cord injury, traumatic brain injury, multiple sclerosis or Parkinson's disease," according to the company. It was released in 2001.
Standard YouTube License @ evolutionofjeff
Janet McCormack - Recovering from a Stroke
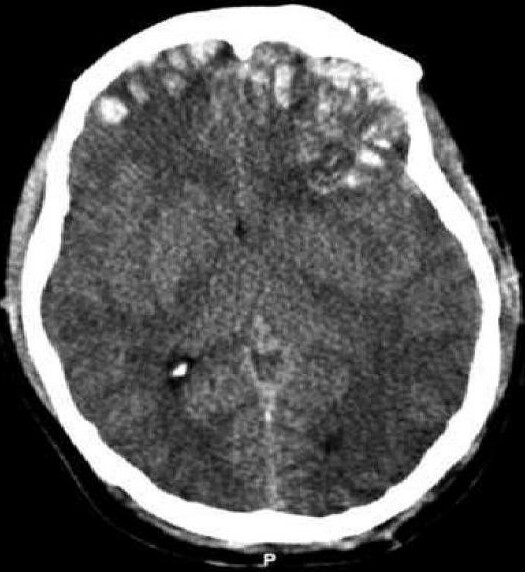
Published on Jul 26, 2012Janet, 32 from Staffordshire who lives with her husband Karl, was participating in an Earls Court Exhibition when she suffered a stroke (intracerebral heamorrhage - ICH).
After major surgery Janet was admitted to the Acute Neurological Rehabilitation Unit at The Wellington Hospital. She was tiring very easily, her balance was very poor, she felt very dizzy and her speech was slurred. As a consequence she was unable to walk unaided and was dependent on help from the nursing staff for washing and dressing.
With the help of the team at the unit Janet set some goals on admission, which said that by discharge she would be able to get herself up and ready in the morning with a little help from her husband. (This included showering and dressing herself and applying her own make up and pinning up her hair).
Janet's rehabilitation programme consisted of Physiotherapy, Nursing, Occupational Therapy, Speech and Language Therapy and Neuropsychology, plus the use of some our latest technology including the Lokomat robotic walking device.
After 3 weeks, Janet was ready to return to Staffordshire to continue her rehabilitation nearer home. Janet had achieved her goal and was beginning to walk with assistance from her husband and was even able to wash her own hair, a huge achievement for her.
Standard YouTube License @ The Wellington Hospital
Lokomat at Madonna Rehabilitation Hospital
Uploaded on Nov 12, 2009Madonna clinicians are currently undergoing intensive training sessions on the use of this cutting-edge piece of robotic equipment, which can help some people improve their ability to walk after disability caused by brain and spinal cord injuries, stroke, or neurological and orthopaedic conditions. Though the Lokomat is an effective and advanced rehabilitation tool, robot-assisted walking therapy is specialized and some medical conditions may limit its appropriateness for all people.
Studies show that locomotion therapy supported by a robotic assisted device on a treadmill is an effective intervention for improving over-ground walking function for those limited by illness or injury. The Lokomats specialized support and limb guidance, and the repetitive walking pattern, help the brain and spinal cord work together to re-route neural pathways, retraining the brain and body to facilitate the gait movements needed for walking.
In addition, Lokomat therapy helps strengthen muscles and improve cardiovascular health. The weight bearing aspect of the Lokomat may aid in the prevention of osteoporosis, building bone mass as the person assumes some of his or her own weight during therapy.
Madonna hopes to begin receiving patient referrals from physicians for the Lokomat in early 2010.
Standard YouTube License @ Madonna Rehabilitation Hospital
The Lokomat Walking Machine
Uploaded on May 7, 2009ARMY.MIL - After the crash of his helicopter, Crew Chief Spc. Mark Lalli is learning to walk again with the aid of an advanced set of robotic legs, a team of doctors, nurses, specialists, and...his mother.
http://www.army.mil/news/health
Standard YouTube License @ U.S. Army
Stephen on Pediatric Lokomat
Uploaded on Nov 9, 2009Stephen receiving Lokomat therapy to learn how to walk. It has worked incredibly well!
Standard YouTube License @ lpluke12
Hocoma's Lokomat in Action
Uploaded on Mar 10, 2009Charles Remsberg, CEO of Hocoma Inc., demonstrates the Lokomat, the first driven gait orthosis that assists walking movements of gait-impaired patients. The Lokomat is used to improve mobility in individuals following stroke, spinal cord injury, traumatic brain injury, multiple sclerosis or other neurological diseases and injuries. For more information on this, and to see other interviews from CSM, visit http://www.therapytimes.com.
Standard YouTube License @ RTImageEdit
Mandell Center: Lokomat
Uploaded on Apr 29, 2009Standard YouTube License @ National MS Society, CT Chapter
Therapy for Spinal Cord Injury in Toronto
Published on Jun 3, 2012Lokomat Therapy, Armeo Therapy, Hyperbaric Oxygen Therapy, Therapy for Stroke, Therapy for SCI, Therapy for Multiple Sclerosis, Therapy for Cerebral Palsy.
Standard YouTube License @ teamtheraputixtv's channel
Locomat Therapy in Toronto Ontario Canada
Published on Mar 13, 2012Advanced Rehabilitation Equipment and Therapies for treating MS, Stroke, Spinal Cord and Traumatic Brain Injuries in Toronto, Canada please visit us at www.theraputix.ca Lokomat Therapy, Armeo Therapy, Hyperbaric Oxygen Therapy
Standard YouTube License @ teamtheraputixtv's channel
Locomat Therapy in Toronto
Published on Mar 13, 2012Advanced Rehabilitation and Therapies for MS, STROKE, SPINAL CORD AND TRAUMATIC BRAIN INJURIES... please visit us at www.theraputix.ca
Standard YouTube License @ teamtheraputixtv's channel
Paralyzed Rats Walk Again
Published on May 31, 2012May 31, 2012 — Scientists in Switzerland have developed a method to help paralyzed rats with severed spinal cords walk — and even climb stairs — again. The team's cocktail of neuron-activating chemicals and electrical stimulation might be a precursor to future treatments for disabled humans, researchers say.
Video courtesy EPFL, Switzerland
Standard YouTube License @ National Geographic
Gabe on the Lokomat
Uploaded on Nov 15, 2011Gabe goes to Theraputix for special therapy on the Locomat machine. Using complex support machinery and biofeedback he is walking his way back to independence.
Standard YouTube License @ Michael Abraham
Learn about the Lokomat.
Published on Jun 26, 2012Lokomat therapy. Learn about the Lokomat. What it is, how it works and meet the therapists.
Standard YouTube License @ Pikeville Medical Center
Lokomat Music Video
Uploaded on Mar 16, 2011A fun way to look at the Lokomat in motion.
A number of videos from various news casts compiled showing success stories and progress from using the Lokomat.
Standard YouTube License @ Aim2Walk